Case Study:
A 59-year old woman traveled 2 hours to my office for a 2nd opinion. She was 5’3 and weighed 252 lbs., down from a peak of 320 lbs. a few years earlier. She had been diagnosed and treated for Type 2 diabetes mellitus since the year 2000 and had been treated for hypertension and hyperlipidemia for a decade. She had been treated once with laser for retinopathy and had mild peripheral neuropathy. She never smoked. Due to progressive kidney failure, she began hemodialysis in 2014 and had a kidney transplant in 2017. She had a carotid endarterectomy in 2016.
She denied angina or dyspnea but underwent a chemical nuclear perfusion scan this year and had moderate to large reversible defects with an ejection fraction of 61%. She underwent right and left heart catheterization showing normal right heart pressures. Her left main was 10% narrowed, her vessels were large, her LAD after a septal branch was 70% narrowed, a first circumflex marginal was functionally occluded 100%, and her distal RCA to a dominant circulation was 80% narrowed. She was advised to have cardiac bypass surgery.
She could ride her stationary bicycle 20 minutes. She used CPAP to sleep. She had followed a whole food plant diet with no added oil on and off over the years, once reaching 180 lbs, and resumed it fully 6 weeks ago. She was down 12 pounds. She worked full time. She had a supportive family nearby. She was on a statin, aspirin, a beta-blocker, nitrates, and diabetic medications.
The ISCHEMIA Trial
One of the most anticipated and expensive trials in the history of cardiology care ($100 million) was presented at the annual American Heart Association meeting in Philadelphia in November, 2019: The ISCHEMIA study. The study design was previously published.
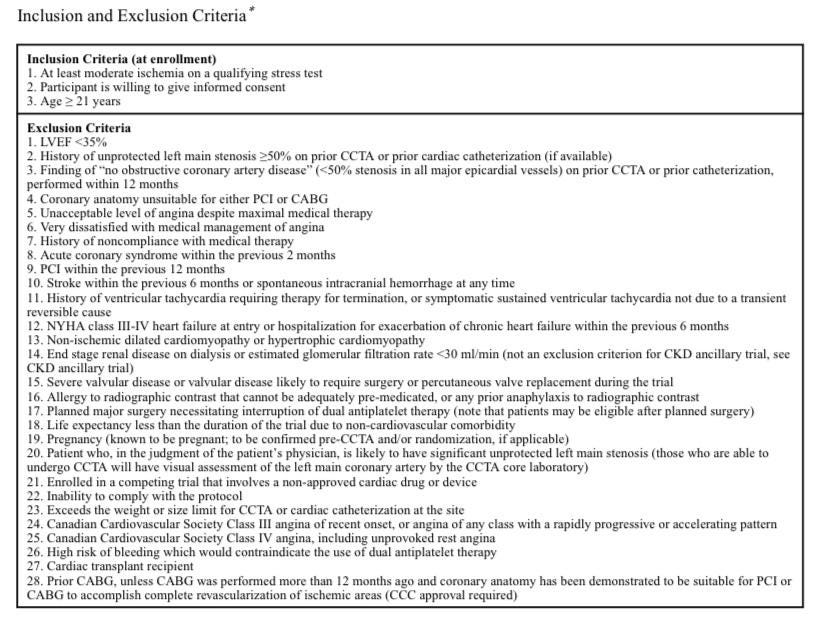
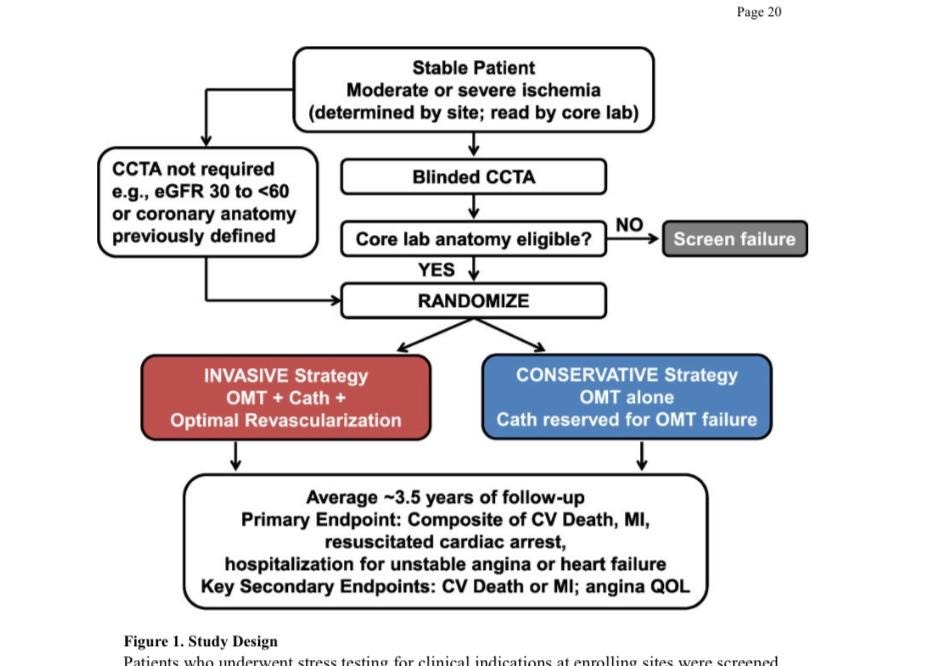
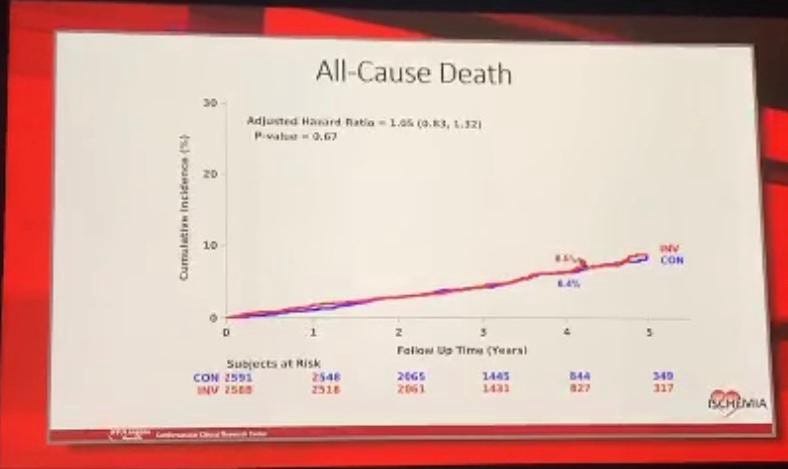
The study randomized 5,197 patients with stable ischemic heart disease (SIHD) identified at a network of international treatment centers with moderate to large zones of ischemia on stress testing in the setting of suspected CAD (just like the case study). Many had a coronary CT angiogram to evaluate for and exclude severe disease of the left main trunk and those without it were randomized to optimal medical therapy and lifestyle changes alone or those therapies plus catheterization. Of those that underwent coronary catheterization, 80% had an intervention. Most were treated with the placement of stents and about 25% were treated with coronary bypass surgery. The subjects were followed for up to 4 years and the results were presented. There were no differences in the 2 groups for overall death rates or cardiovascular death rates. The primary composite end point was not significantly different between the 2 groups. As was summarized by the American College of Cardiology (ACC):
“Results showed that the cumulative incidence of the primary endpoint — a composite of cardiovascular death, MI, resuscitated cardiac arrest, or hospitalization for unstable angina or heart failure — was 15.5 percent in the conservative group vs. 13.3 percent in the invasive group after 4 years. In addition, the cumulative incidence of the major secondary endpoint — cardiovascular death or MI — was 13.9 percent in the conservative group vs. 11.7 percent in the invasive group after 4 years”.
A subgroup of 777 patients enrolled with chronic kidney disease, usually viewed as higher risk, was also presented. As summarized by the ACC,
“Results showed that the cumulative incidence of the primary endpoint — a composite of death or nonfatal MI — was 36.7 percent in the conservative group vs. 36.4 percent in the invasive group after 3 years. In addition, the cumulative incidence of the major secondary endpoint — a composite of death, nonfatal MI, hospitalization for unstable angina, hospitalization for heart failure, or resuscitated cardiac arrest — was 39.7 percent in the conservative group vs. 38.5 percent in the invasive group after 3 years”.
How Were the Medical Therapy Patients Treated?
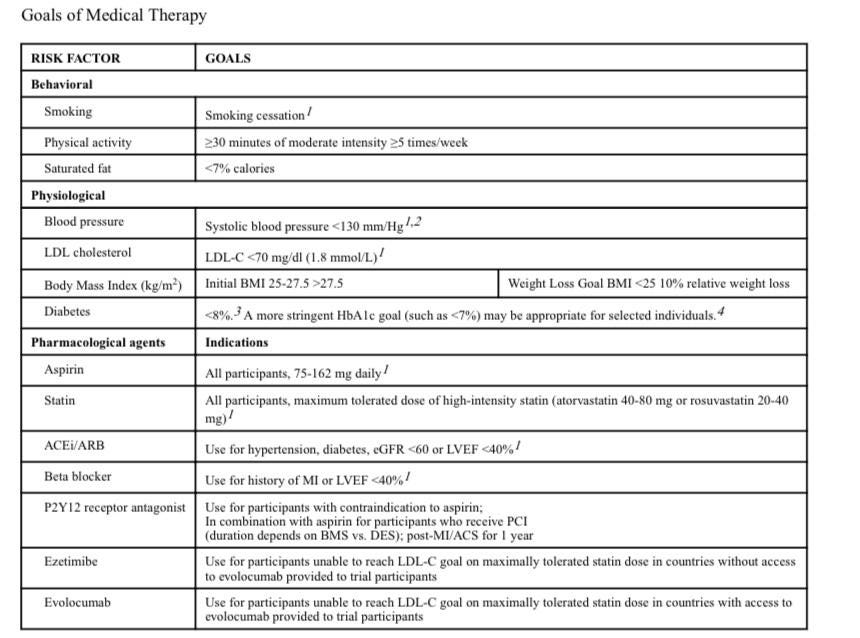
The study design for the ISCHEMIA trial has been published and shown below. Called Optimal Medical Therapy (OMT), it was based on a diet low in saturated fat, regular fitness activities, and optimal medications. It did not apply the proven benefits of a more comprehensive program paid for by Medicare and other insurers called intensive cardiac rehabilitation (ICR) as reported by Dean Ornish, MD and the Pritkin Longevity Center. The patient in the case study had met and exceeded the OMT goals of the ISCHEMIA trial.
How Should the Case Study Patient be Treated?
The woman I saw had no angina. She met the stress test criteria for the ISCHEMIA trial. She was on or exceeded the OMT guidelines of the study. She was advised by her local medical team to have coronary bypass surgery but was at increased risk due to her renal disease, short stature, obesity and carotid disease.
In my second opinion consult I reviewed with her all the data above and presented her the option to proceed with surgery or OMT. I advised her that it takes a strong patient committed to diet and fitness to “stand up” to her local medical team. I warned her they might refuse to treat her if she declined their recommendations (the sad truth). I offered her a prescription for cardiac rehabilitation in her community.
She is contemplating the options but is on her path to avoid a cardiac operation that offers her no advantage for quality of life or lifespan. What would you do?







